Sophisticated HIS-RIS-PACS Integration in a large scale traumatology PACS
S. Peer (1), R. Vogl (2), R. Peer (1), W. Jaschke (1)
(1) University of Innsbruck, Department of Radiology
(2) TILAK-GesmbH, Department of Information Managment
Introduction:
Radiology in the context of an outpatient trauma care centre demands high technical as well as logistical expertise. Rapid image acquisition and immediate distribution of all necessary patient x-rays as well as reports to the surgeon is the foremost aim. In the context of a PACS-installation this task can only be met with in depth analysis of the workflow within the radiology as well as traumatology department and transfer of the desired workflow onto the digital environment by sophisticated integration of all involved electronical information systems.
System description:
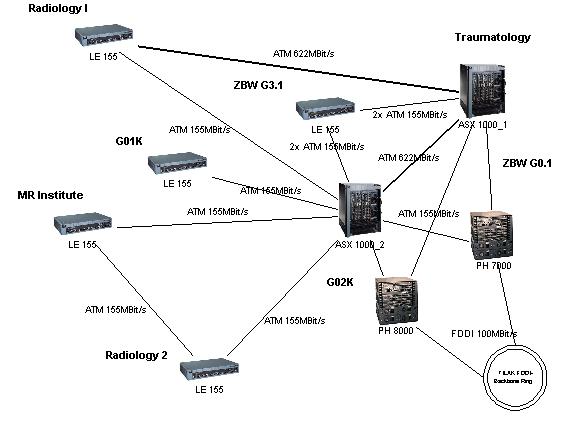
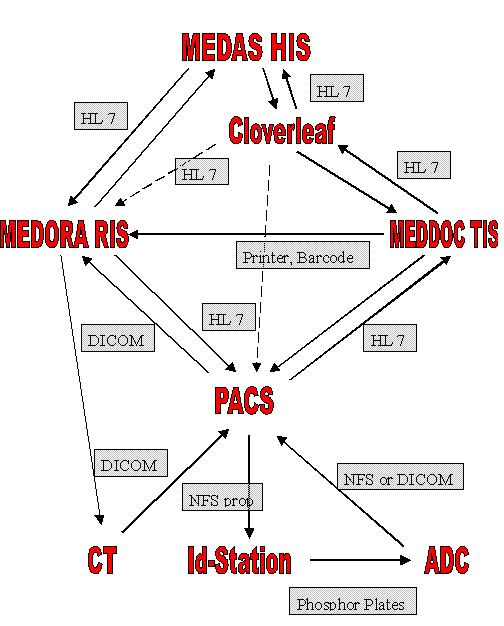
The traumatology PACS in Innsbruck is based on a fast ATM-network in star topology. Included are 3 AGFA ADC70 storage phosphor radiography units, a GE helical CT-scanner, an ATL HDI 5000 ultrasound unit, a Phillips Integris angiography unit, a Lumisys x-ray film scanner and 28 workstations. As a general rule all images in the short term as well as long term archive are available to every single user on every workstation within the network at any time. The patient is normally registered or scheduled via the TIS (which also directs the prefetching) or RIS where patient data are cross checked with the HIS via an HL7-interface. Patient data and the information about the requested x-rays from the TIS are then handed over to the PACS-server via HL7 and electronically printed on a laser printer in the x-ray department (to inform the radiology technician and to read the data into the RIS via a barrcodelaser) and then distributed to the AGFA identification terminals or the CT-console via a DICOM-worklist function. Acquired images are sent to the PACS archive immediately (and thus accesible for every user at the same time) and a study content notification is sent to the RIS (via DICOM) and UIS (via HL7) simultaneously. Changes in the patient status or in patient data are transfered to the TIS, RIS and PACS from the HIS via HL7.
Results:
The implementation of the workflow was difficult, as the PACS has to serve two clients directly.
Identical organisational structures had to be implemented in both departmental information systems to guarantee for complete functionality in both systems. By the implemented workflow input of patient data or imaging data by hand can be kept to a minimum (normally only once) which is critical to avoid misregistrations and thus falsley arranged or archived imaging data in the PACS.
 |
 |
Discussion:
In the implemented configuration the aim of rapid image and report distribution to the surgeon without interaction of the radiology staff was reached. Adherence to industrial standards (DICOM, HL7) allows for complex workflow interactions. While DICOM allows for data distribution between subsystems, the way these data are provided within the standard may differ, why individual adaptations have to be made. Continuous workflow analysis by a dedicated team of radiologists, surgeons and technical staff proved to be key for the succes of the project.
Corresponding author:
Dr. Siegfried Peer
Dept.of Radiology, University Hospital
Anichstr.35
A-6020 Innsbruck, Austria
Tel.: 0043/512/504/2761
E-Mail: Siegfried.Peer(at)uibk.ac.at
Oral presentation at EuroPACS'98, Barcelona, Spain